Neoadjuvant therapy is a treatment approach used for
pancreatic cancer that involves administering chemotherapy and/or radiation
therapy before the main treatment, which is usually surgery. The goal of
neoadjuvant therapy is to shrink the tumor, potentially making it more operable
or improving the chances of a successful surgical outcome. It can also help to
identify how the tumor responds to treatment and provide valuable information
for further treatment planning. Neoadjuvant therapy for pancreatic cancer
typically involves a combination of chemotherapy and radiation therapy,
although the specific treatment plan may vary based on individual patient
factors and the stage of the cancer.
Advantages
Neoadjuvant therapy for pancreatic cancer offers several
advantages, including:
1. Downstaging
the tumor: Neoadjuvant therapy aims to shrink the tumor before surgery. This
downstaging can potentially make the tumor more operable, allowing for a more
successful surgical resection. It may convert initially unresectable tumors
into resectable ones, increasing the likelihood of a curative surgery.
2. Increasing
the chance of complete tumor removal: By reducing the size of the tumor,
neoadjuvant therapy can help improve the chances of achieving clear surgical
margins. Complete removal of the tumor with negative margins (no cancer cells
at the edges) is crucial for better long-term outcomes.
3. Treating
micrometastases: Pancreatic cancer often has a high likelihood of spreading to
other parts of the body even before it is diagnosed. Neoadjuvant therapy can
target these micrometastases (small clusters of cancer cells) that may be
present but undetectable at the time of diagnosis. This may help prevent or
control distant metastasis.
4. Assessment
of tumor response: Neoadjuvant therapy allows physicians to assess how the tumor
responds to treatment. This can provide valuable information on the tumor's
biology, sensitivity to specific therapies, and overall prognosis. It helps
guide further treatment decisions and may indicate the need for additional
adjuvant therapy after surgery.
5. Tailoring
treatment plans: The response to neoadjuvant therapy can help personalize the
treatment approach. If the tumor shows a favorable response, it may indicate
that a particular chemotherapy regimen is effective, guiding subsequent
adjuvant therapy. Conversely, if the tumor is resistant to neoadjuvant
treatment, alternative strategies can be explored, such as different
chemotherapy combinations or targeted therapies.
6. Potentially
increasing the likelihood of survival: Some studies suggest that neoadjuvant
therapy may improve survival rates for pancreatic cancer patients. By attacking
the tumor before surgery and addressing any potential micrometastases, it may
help control the disease more effectively and reduce the risk of recurrence.
Limitations
While neoadjuvant therapy for pancreatic cancer offers
several advantages, there are also some limitations and considerations to be
aware of:
1. Tumor
resistance: Not all tumors respond favorably to neoadjuvant therapy. Some
tumors may be inherently resistant to chemotherapy or radiation, leading to
limited or no shrinkage. In such cases, the benefits of neoadjuvant therapy may
be limited, and alternative treatment approaches may need to be explored.
2. Delay
in definitive treatment: Neoadjuvant therapy typically involves several weeks
of chemotherapy and/or radiation before surgery. This can result in a delay in
the initiation of the definitive treatment, which is surgical resection. For
some patients with rapidly progressing tumors, delaying surgery may not be the
optimal choice.
3. Disease
progression during neoadjuvant therapy: In some cases, pancreatic cancer may
progress during neoadjuvant therapy. Tumors may become more aggressive or
develop resistance to the treatment, making them unresectable or limiting the
benefits of surgery. Regular monitoring and evaluation during neoadjuvant
therapy are essential to identify disease progression and adjust the treatment
plan accordingly.
4. Surgical
complications: Although neoadjuvant therapy aims to improve surgical outcomes,
it does not eliminate the risks associated with surgery. Pancreatic surgery is
complex and carries potential risks, including bleeding, infection, organ
damage, and postoperative complications. The decision to proceed with surgery
after neoadjuvant therapy must carefully consider the patient's overall health
and surgical risks.
5. Patient
selection: Neoadjuvant therapy is not suitable for all patients with pancreatic
cancer. Factors such as overall health, tumor stage, and patient preferences
must be considered when determining the appropriateness of neoadjuvant therapy.
Some patients may not tolerate the side effects of chemotherapy or radiation,
making it necessary to explore alternative treatment options.
6. Lack
of standardized protocols: Neoadjuvant therapy for pancreatic cancer is still
an evolving field, and there is no standardized protocol. The optimal
chemotherapy regimens, radiation techniques, and timing of surgery are still
being investigated and may vary among healthcare institutions. This lack of
standardization can lead to variations in treatment approaches and outcomes.
Protocol
The protocol for neoadjuvant therapy in pancreatic cancer
may vary depending on factors such as tumor stage, patient characteristics,
institutional guidelines, and the preferences of the healthcare team. However,
a common approach to neoadjuvant therapy for pancreatic cancer typically
involves a combination of chemotherapy and radiation therapy. Here is a general
outline of the protocol:
1. Chemotherapy:
·
Typically, a combination chemotherapy regimen is
used. One commonly used regimen is FOLFIRINOX, which includes a combination of
four drugs: 5-fluorouracil (5-FU), leucovorin, irinotecan, and oxaliplatin.
Another regimen is gemcitabine-based chemotherapy, either as monotherapy or in
combination with nab-paclitaxel.
·
The duration and number of chemotherapy cycles
may vary, but a standard approach involves administering chemotherapy for
several months before surgery. The exact duration and number of cycles are
determined based on individual patient factors and tumor response to treatment.
2. Radiation
therapy:
·
External beam radiation therapy is commonly used
in neoadjuvant protocols. It involves directing high-energy X-rays or other
radiation sources to the tumor and surrounding tissues.
·
The purpose of radiation therapy is to target
and shrink the tumor, making it more amenable to surgical resection. It may
also help in controlling micrometastases and reducing the risk of local
recurrence.
·
Radiation therapy is typically administered
concurrently with chemotherapy, either throughout the entire course of
chemotherapy or during specific cycles.
·
The total radiation dose and number of fractions
delivered may vary depending on the specific treatment plan and institutional
guidelines.
3. Evaluation
and monitoring:
·
Regular imaging tests, such as computed
tomography (CT) scans, are performed during neoadjuvant therapy to monitor the
tumor response to treatment.
·
Response evaluation is essential to assess the
tumor's downstaging, identify potential disease progression, and guide
treatment decisions.
4. Surgical
resection:
·
After completion of neoadjuvant therapy,
patients are reevaluated to determine if they are suitable candidates for
surgery.
·
The decision for surgical resection is based on
factors such as tumor response, absence of distant metastasis, and overall
patient health.
·
Surgical procedures may include a
pancreaticoduodenectomy (Whipple procedure), distal pancreatectomy, or other
specialized techniques, depending on the location and extent of the tumor.
·
Postoperative treatment, such as adjuvant
chemotherapy, may be considered depending on the individual patient's
characteristics and the pathology findings.
History
Neoadjuvant therapy for pancreatic cancer has gained
recognition and acceptance over the past few decades. Here is a brief overview
of the history of neoadjuvant therapy in pancreatic cancer:
1. Emergence
of chemotherapy: In the 1980s, the use of chemotherapy in pancreatic cancer
began to gain prominence. Gemcitabine, a chemotherapy drug, was introduced in
the late 1990s and became the standard treatment for advanced pancreatic
cancer.
2. Studies
on neoadjuvant therapy: In the early 2000s, studies started investigating the
potential benefits of neoadjuvant therapy in pancreatic cancer. These studies
aimed to determine if administering chemotherapy or chemoradiotherapy before
surgery could improve outcomes compared to upfront surgery alone.
3. Early
clinical trials: Initial clinical trials focused on evaluating the feasibility
and safety of neoadjuvant therapy in pancreatic cancer. These trials
demonstrated the potential to achieve tumor downstaging, improve surgical
resectability, and control micrometastatic disease.
4. PRODIGE
and PREOPANC trials: Two pivotal studies, PRODIGE 4/ACCORD 11 and PREOPANC-1,
published in 2009 and 2018 respectively, played a significant role in
establishing neoadjuvant therapy as a viable approach. These trials
demonstrated improved outcomes with neoadjuvant treatment compared to upfront
surgery alone in terms of increased R0 resection rates (complete tumor
removal), prolonged survival, and improved disease-free survival.
5. Evolution
of chemotherapy regimens: With the success of neoadjuvant therapy, different
chemotherapy regimens have been explored. FOLFIRINOX, a combination regimen of
5-fluorouracil (5-FU), leucovorin, irinotecan, and oxaliplatin, has shown
superior efficacy compared to gemcitabine-based regimens. It has become a
preferred choice for neoadjuvant treatment in eligible patients.
6. Clinical
practice guidelines: Leading professional organizations, such as the National
Comprehensive Cancer Network (NCCN) and the European Society for Medical
Oncology (ESMO), now recommend considering neoadjuvant therapy as a treatment
option for selected patients with resectable or borderline resectable pancreatic
cancer.
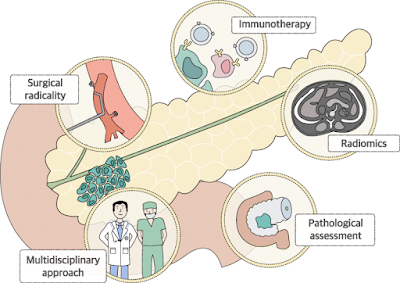
Research
Research in neoadjuvant therapy for pancreatic cancer is
ongoing, with studies focusing on refining treatment protocols, exploring
targeted therapies, immunotherapies, and personalized approaches. The aim is to
further improve outcomes, identify predictive biomarkers, and optimize
treatment strategies for individual patients.
Ongoing research in the field of neoadjuvant therapy for
pancreatic cancer aims to further improve treatment outcomes, refine treatment
strategies, and explore novel therapeutic approaches. Here are some areas of
ongoing research:
1. Optimization
of chemotherapy regimens: Researchers are investigating different chemotherapy
regimens, combinations, and dosing schedules to enhance the effectiveness of
neoadjuvant therapy. Studies are evaluating the use of modified FOLFIRINOX
regimens, gemcitabine-based combinations, and other novel agents to improve
response rates and minimize side effects.
2. Targeted
therapies: Targeted therapies that specifically inhibit molecular pathways
involved in pancreatic cancer progression are being studied. These therapies
aim to improve tumor response and patient outcomes. Examples include targeted
agents against the epidermal growth factor receptor (EGFR), vascular
endothelial growth factor (VEGF), and immune checkpoint inhibitors.
3. Immunotherapy:
Immunotherapy, such as immune checkpoint inhibitors, is being explored in
neoadjuvant settings. Researchers are investigating the use of immunotherapies
to enhance the immune response against pancreatic cancer and improve treatment
outcomes. Clinical trials are evaluating immune checkpoint inhibitors, adoptive
T-cell therapies, and therapeutic cancer vaccines.
4. Biomarkers
and predictive markers: Researchers are seeking reliable biomarkers and
predictive markers to identify patients who are most likely to benefit from
neoadjuvant therapy. By identifying biomarkers associated with treatment
response, researchers aim to personalize treatment strategies and improve
patient selection.
5. Radiogenomics
and imaging techniques: Radiogenomics is a field that explores the relationship
between genomic characteristics of tumors and imaging features. Researchers are
investigating the use of radiogenomics and advanced imaging techniques, such as
functional MRI, diffusion-weighted imaging, and positron emission tomography
(PET), to predict treatment response, assess tumor biology, and guide treatment
decisions.
6. Liquid
biopsies: Liquid biopsies involve the analysis of circulating tumor DNA (ctDNA)
or other biomarkers present in blood samples. Researchers are exploring the
utility of liquid biopsies in pancreatic cancer to monitor treatment response,
detect minimal residual disease, and identify potential resistance mechanisms.
This non-invasive approach may help in treatment decision-making and monitoring
treatment effectiveness.
7. Integration
of neoadjuvant therapy with other modalities: Studies are investigating the
optimal sequencing and combination of neoadjuvant therapy with other treatment
modalities, such as radiation therapy, targeted therapies, and immunotherapies.
The goal is to develop comprehensive treatment strategies that maximize
treatment response and long-term outcomes.
These ongoing research efforts aim to advance the field
of neoadjuvant therapy for pancreatic cancer and improve patient outcomes. It
is important for patients to discuss potential participation in clinical trials
with their healthcare team to explore novel treatment options and contribute to
the advancement of pancreatic cancer care.